
Get breaking news alerts and special reports. The news and stories that matter, delivered weekday mornings.
Drug-resistant superbugs, already a big problem in hospitals, may have learned a new trick, researchers reported Wednesday.
They may have evolved resistance to alcohol — the ingredient in hand sanitizers and disinfectants that are one mainstay of hospital infection control, Australian researchers said.
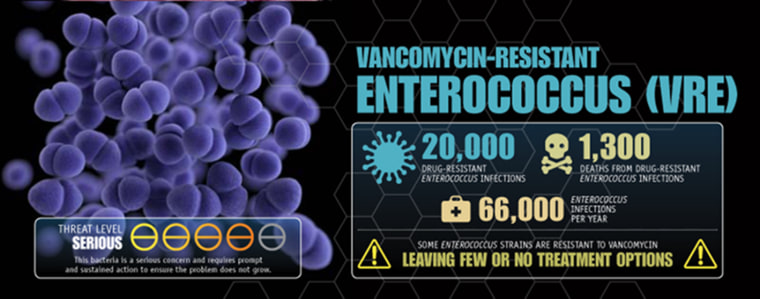
A 3D image of a cluster of paired vancomycin-resistant enterococcus bacteria. James Archer / U.S. Centers for Disease Control and Prevention
If true, it could be even harder than it already is to control the spread of infection in hospitals, the researchers wrote in the journal Science Translational Medicine.
If bacteria can evade the effects of alcohol, it will come as a surprise to many microbiologists, who have assumed that it could not happen. While bacteria can evolve the ability to resist antibiotics, for instance by pumping them out, alcohol kills more efficiently.
The team at the Peter Doherty Institute for Infection and Immunity in Melbourne identified and studied a strain of vancomycin-resistant enterococci called Enterococcus faecium. It is a common hospital nuisance and while not particularly deadly, it can make hospitalized patients even sicker. (Vancomycin is an antibiotic used to treat bacterial infections.)
“The development of alcohol-tolerant strains of E. faecium has the potential to undermine the effectiveness of alcohol-based disinfectant standard precautions and may, in part, explain the increase in VRE infection that is now widely reported in hospitals in Europe, Asia, the Americas, and Australia,” they wrote in their report.
The World Health Organization says antibiotic-resistant bacteria are a “fundamental threat” and has made fighting them a priority.
The Centers for Disease Control and Prevention estimates that 23,000 Americans die every year from drug-resistant infections.
The need to battle the spread of these germs is the reason why people are constantly reminded to wash their hands and why dispensers of alcohol foam or gel have appeared everywhere in hospitals and in other public spaces.
But the Australian team said their findings indicate that people will have to be careful how they use these hand sanitizers.
They started their study a few years ago, after Australia began a hand sanitizer campaign.
 Vancomycin-resistant enterococci are a major hospital nuisance.U.S. Centers for Disease Control and Prevention
Vancomycin-resistant enterococci are a major hospital nuisance.U.S. Centers for Disease Control and Prevention
In a video released by the Doherty Institute, Dr. Paul Johnson, an infectious-diseases specialist, said the team wanted to know why a superbug known as MRSA, methicillin-resistant Staphylococcus aureus, was being so well controlled with the new national hand hygiene.
“But we started to notice also a gradual increase in VRE infections and this seemed like a paradox because both infections should be controlled using standard hand hygiene.”
They ran a series of experiments, including one in which they took old samples of VRE dating back to 1997, and new samples from 2015, and grew them in dishes with diluted alcohol. The newer samples grew better.
“We were also able to identify and document the specific genetic changes that have occurred in the bacteria over the 20 years, which also helps to explain the increased tolerance,” microbiologist Tim Stinear of the University of Melbourne, who helped lead the study team, said in a statement.
Not everyone is sold on the idea.
“The jury’s still out as to whether this should raise a major alarm,” said Dr. Cindy Liu, chief medical officer of the Antibiotic Resistance Action Center at George Washington University.
The report “doesn’t seem like it could fully explain what is going on,” added Liu, who was not involved in the research.
Nevertheless, she said, the study did seem to show that bacteria can survive in low concentrations of alcohol, which would provide a good reason for people to be more careful in using hand sanitizers. “The effectiveness of the alcohol depends on how you apply it,” Liu told NBC News.
The Australian team said hospitals sometimes use hand sanitizers with two different germ-killing compounds, such as alcohol and chlorhexidine. That may be a better strategy going forward, they said. And they noted that foams and gels tend to be less effective at killing germs than liquids.
Liu agreed. Just as with washing hands with soap and water, it takes time to kill germs using hand sanitizers. People may not realize that they must thoroughly soak their hands. “You have to leave them on at least 30 seconds,” she added.
Be the first to comment